ANS Part II: Receptors, transmitters and drugs
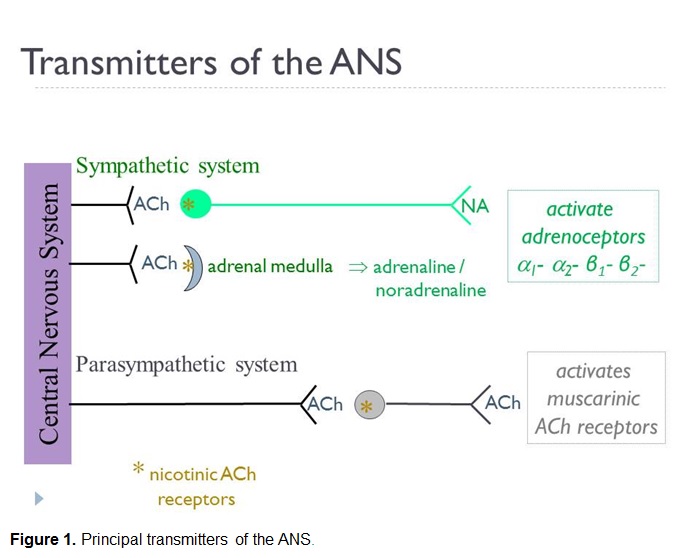
The two principal (or 'classical') small transmitter molecules used by neurons of the motor ANS are acetylcholine (ACh) and noradrenaline (NA). Many others, some of which will be mentioned in other sections [e.g. adenosine triphosphate (ATP), nitric oxide (NO) and numerous peptides], act as co-transmitters, or modulators. See Figure 1 below.
The key facts, which are summarised in Box 1, are:
- all preganglionic neurons, sympathetic and parasympathetic, are cholinergic, meaning that they synthesise and release ACh as their primary transmitter. Thus, fast synaptic neurotransmission at the autonomic ganglia is always mediated by ACh.
- all postganglionic neurons communicate with their effector targets by chemical transmission at neuroeffector junctions. The latter are generally not regarded as conventional synapses because they lack structural elements of, for example, the best studied synapse, that of the skeletal neuromuscular junction. Moreover, each axon has sites of transmitter release from multiple swellings, known as varicosities, which occur along its distal portion, giving a 'string of pearls' appearance. The distance between the varicosity and postjunctional membrane, through which transmitter must diffuse, varies greatly between the innervated tissues (the extremes being 20 nm to 1-2 µm) and is generally much wider than the cleft at a synapse such as the skeletal neuromuscular junction (~ 30 nm).
- parasympathetic postganglionic neurones are mainly cholinergic, releasing ACh at the neuroeffector junction. In some instances a gas, nitric oxide (NO) may subserve neurotransmission.
- sympathetic postganglionic postganglionic neurones are largely adrenergic, meaning that they synthesise and release NA as their primary transmitter. It should be noted that that NA is also known as norepinephrine (NE), particularly in North America. Fortunately, 'norepinephrinergic' (which is an abomination to Pharmacologists!) is not used as an alternative nomenclature to adrenergic. ATP is frequently released with NA as a co-transmitter. A minority of sympathetic postganglionic neurones, such as those innervating eccrine sweat glands, are cholinergic.
- As is generally the case in chemical neurotransmission, the release of either ACh, or NA, from presynaptic or prejunctional sites is triggered by the arrival of an action potential. The latter evokes membrane depolarization that in turn opens voltage-activated calcium-selective ion channels that allow influx of Ca2+. The resultant local increase in intracellular Ca2+ concentration causes vesicles in which the transmitter is stored to fuse with the presynaptic/prejunctional membrane liberating the transmitter to activate postsynaptic/postjunctional receptors. Such release of transmitters from vesicles in response to Ca2+ is known as exocytosis.
- The most important receptors through which the autonomic transmitters act, at least from the perspective of current therapeutic agents, are cholinoceptors and adrenoceptors that are activated by ACh and NA (or adrenaline), respectively. Still others to be introduced in other sections mediate the effects of co-transmitters and modulators of the ANS. Nitric oxide has the distinction of acting via an enzyme (soluble guanylyl cyclase), rather than a receptor.
- The cholinoceptors are fundamentally classed as nicotinic, which are ligand-gated ion channels (LGICs), or muscarinic which are G-protein-coupled receptors (GPCRs). This nomenclature is rooted deeply in the history of Pharmacology, the plant alkaloids nicotine and muscarine being the earliest studied selective agonists of nicotinic and muscarinic cholinoceptors, respectively. A large number of antagonists, some of which are of past, or current, therapeutic importance are also strongly selective between skeletal neuromuscular junction nicotinic (e.g. vecuronium), ganglionic nicotinic (e.g. hexamethonium) and muscarinic (e.g. atropine) cholinoceptors.
- Both nicotinic and muscarinic receptors exist as multiple subtypes. The structural underpinnings of such diversity will be mentioned in other sections, but for now it is sufficient to note that the nicotinic receptors of the ganglia and skeletal neuromuscular junction, which many Physiology texts unhelpfully (and in violation of NC-IUPHAR nomenclature recommendations!) denote NN (or N2) and NM (or N1) respectively, are pharmacologically distinct which is of clinical importance). For example, a very common task of the anaesthetist is to reversibly block the nicotinic receptors of the skeletal neuromuscular junction to achieve controlled paralysis without perturbing transmission through the ganglia by blocking ganglionic nicotinic receptors. Muscarinic receptors exist as five subtypes: M1, M2, M3, M4and M5 with differing tissue/organ locations and hence physiological functions. Efforts to develop clinically useful subtype-selective antagonists of muscarinic receptors, which we will see is a highly desirable goal, have thus far met with limited success, largely due to the structural conservation of the orthosteric site to which the transmitter, ACh, binds. Pirenzepine and solifenacin are examples of antagonists with marginal selectivity for M1 and M3 receptors, respectively, whilst atropine (above) is non-selective.
Adrenoceptors also exist as numerous subclasses. A fundamental distinction is between α- and β-adrenoceptors, first made by careful study of the rank order of potency of agonists including NA, A and isoprenaline (aka isoproterenol), a synthetic agent. Subsequently, α1-, α2-, β1-, β2- and β3-adrenoceptors have been characterised structurally and pharmacologically. Such receptors have distinct tissue/organ locations (e.g. β1 - cardiac nodes and muscle; β2 - airway smooth muscle) and drugs that selectively activate (e.g. salbutamol, aka albuterol - a β2 agonist) and block (e.g. atenolol - a β1 antagonist) adrenoceptor subtypes are some of the most important and frequently used drugs in medicine.
| Box 1. Comparison of the Sympathetic and Parasympathetic Divisions of the Motor Autonomic Nervous System | ||
|---|---|---|
| Sympathetic | Parasympathetic | |
|
Location of preganglionic neurone cell body |
Thoracolumbar spinal cord |
Brainstem, sacral spinal cord |
|
Length of preganglionic fibre and fibre class |
Short, mostly motor B-myelinated |
Long, mostly motor B-myelinated |
|
Principal transmitter of preganglionic neurones and receptor of postganglionic neurones |
Acetylcholine (ACh), ganglionic nicotinic cholinoceptor |
Acetylcholine (ACh), ganglionic nicotinic cholinoceptor |
|
Location of autonomic ganglia |
Prevertebral as sympathetic chains on either side of the spinal cord and paravertebral within the abdomen |
Discrete ganglia within the head, pelvic ganglia, or intramural ganglia within walls of target organs |
|
Length of postganglionic fibre and fibre class |
Long, motor C-unmyelinated |
Short, motor C-unmyelinated |
|
Principal transmitter of postganglionic neurones and receptor on post-junctional cells |
noradrenaline (NA) (occasionally ACh), α- and β-adrenoceptors and their subclasses (occasionally muscarinic cholinoceptors) |
acetylcholine (ACh), muscarinic cholinoceptors |
|
Established co-transmitters, or modulators* |
adenosine triphosphate (ATP), neuropeptide Y |
nitric oxide (NO), vasoactive intestinal peptide (VIP) |
|
Examples of receptor agonists mimicking neuroeffector transmission that are in clinical use** |
phenylephrine (α1-adrenoceptor selective) |
bethanechol (muscarinic, non-selective) |
|
Examples of receptor antagonists blocking neuroeffector transmission that are in clinical use** |
doxazosin (α1-adrenoceptor selective) atenolol (β1-adrenocptor selective) |
atropine (muscarinic, non-selective) |
|
* Neurotransmission mediated by transmitters other than ACh and NA is termed non-adrenergic non-cholinergic (NANC) and includes nitrergic (NO), purinergic (e.g. ATP) and peptidergic (numerous peptides, including VIP). **Only a few exemplar drugs are listed. A more comprehensive listing is given in sections on the sympathetic and parasympathetic nervous systems. |
||
An overview of the transmitters and receptors of the ANS is available here.
While acetylcholine and noradrenaline are considered the major transmitters of the autonomic nervous system, non-adrenergic, non-cholinergic (“NANC”) nerves which release transmitters such as nitric oxide (NO) and ATP have also been identified. These NANC transmitters are co-localised and released with the main transmitter and may act to modulate its action or act as co-transmitters, contributing to the response seen with nerve activation. Indeed in some tissues, the NANC transmitter may be the major transmitter (for example nitric oxide (NO) in the male genitourinary tract).
Pharmacologic modulation of the ANS
Drugs can modulate the activity of the autonomic nervous system by interacting at a number of different sites and the range of effects caused will vary depending on how many systems will be affected. As mentioned above, drugs which interfere with ganglionic transmission will affect the outflow of both the sympathetic and parasympathetic systems. However, drugs which target the receptors in the effector tissues, particularly if they are selective for subtypes of receptors, will have the greatest selectivity and fewer unwanted effects.


This 23 slide Powerpoint presentation is intended to introduce the reader to the function of the autonomic nervous system (ANS). Specific areas that are covered include: the basic organization of the motor ANS and its components; the sympathetic and parasympathetic outflows from the central nervous system (CNS) to peripheral organs: the basics of neurochemical neurotransmission within the motor ANS including key neurotransmitters and receptor types; important selected activities of the motor ANS and finally some misconceptions regarding the ANS that even the beginner should be aware of.